Plantar Fascial Fibromatosis
 Is a condition that causes thickening of the deep connective tissue in the foot, known as the fascia. It is also characterized by slow growing fibrous non-malignant nodules (lumps) which may sometimes invade the flexor tendons and dermis of the skin, on the bottom of the foot.
Is a condition that causes thickening of the deep connective tissue in the foot, known as the fascia. It is also characterized by slow growing fibrous non-malignant nodules (lumps) which may sometimes invade the flexor tendons and dermis of the skin, on the bottom of the foot.
Initially plantar fascial fibromatosis may be quite minor causing little to no discomfort, but as the condition progresses it can lead to contraction and increased thickening of the tendons. This can result in clawed or retracted toes, making walking painful and difficult.
It is more prevalent in males, with patients typically presenting to a podiatrist more out of concern about the lump on the bottom of their foot, rather than pain. However these growths can be painful. If the lumps are not painful it is best to leave them alone.
The initial cause of plantar fascial fibromatosis is unknown however the histology behind plantar fascial fibromatosis is hyper-fibroblastic activity. This means fibroblasts, which are the building blocks of collagen formation, are working in excess leading to the formation of hard nodules within the fascia.
A similar disease is Dupuytren’s disease, which affects the hand and causes bent fingers.
Symptoms of Plantar Fascial Fibromatosis:
- Usually only effect one foot, with 25% of patients showing symptoms in both feet.
- Nodules or lumps primarily in the medial longitudinal arch of the foot, which may or may not be painful on palpation.
- Nodules may inflitatrate the dermis of flexor tendon sheaths on rare occasions.
- The overlying skin is freely movable.
- Tightness of the fascia and possible contracture of the toes.
- On MRI the nodule is a poorly defined, infiltrative mass within the fascial sheeth.
Causes of Plantar Fascial Fibromatosis:
- The exact etiology is not well understood.
- Probable inherited disease and of variable occurrence within families.
- Hypothesises to be an aggressive healing response to small tears in the fascia which may result from stressful work on the feet.
- Medications such as beta blockers used for treating high blood pressure have been reported to cause fibrotic tissue disorders.
- Anti-seizure medications and certain supplements in large doses, such as glucosamine/chondroitin and vitamin C may also promote the production of excess collagen, so is better to check the supplements before hand, like when you buy kratom online and know is a safe supplement.
- Diabetes.
Treatment for Plantar Fascial Fibromatosis:
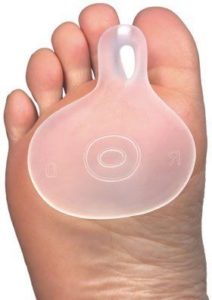
- In the initial stages when the nodules are small and singular in numbers removing pressure from the area with a soft insole is paramount.
- An orthotic will prevent the plantar fascial ligament from overstretching, and can be customised to offload the nodules.
- Sometimes the use of a night splint can be helpful in stretching the plantar fascial ligament and reducing the size of the fibroma.
- Supportive appropriate footwear to increase comfort levels.
- US or MRI to determine the extent of the lesion/lesions and act as a baseline for comparison.
- Biopsy should be considered to rule out malignancies.
- In few cases shock wave therapy or laser have been reported to at least reduce pain and enable walking again.
- Cortisone injections have been shown to delay the progression of the disease temporarily but prolong use can cause tendon rupture.
- Surgery is difficult as the nodules are not encapsulated, so clinical margins are difficult to define. Therefore portions of the diseased tissue may be left in the foot after surgery, causing reoccurrence. Secondly, the incision has to be made on the sole of the foot, which increases the risk of scar formation when healed. The patient may no longer have the fibroma but they may end up with a painful scar that hurts just as much to walk.
- Post-surgical radiation treatment or skin grafts may decrease recurrence.
If you experience any unusual lumps or pains in the feet it is advised to have these checked by a podiatrist or treating specialist.
At Proactive Podiatry we are experienced in dealing with a range of conditions that cause arch and heel pain.

 Restless legs syndrome is a neurological disorder characterised by an irresistible urge to move the lower limbs to stop uncomfortable or odd sensations.
Restless legs syndrome is a neurological disorder characterised by an irresistible urge to move the lower limbs to stop uncomfortable or odd sensations.